Patient deductibles reset to zero every January 1st. Here's how to prepare your verification workflows and avoid revenue leakage.
Every December 31st, the clock strikes midnight and something quietly catastrophic happens to your revenue cycle: patient deductibles reset to zero, out-of-pocket accumulators vanish, and that patient who paid $25 per visit last month? They now owes $150 or more until their new deductible is satisfied.
The January deductible reset is exactly what it sounds like: the moment when most patients' annual insurance benefits restart fresh on January 1st. All those dollars they spent working toward their deductible last year? Gone, they're starting over at zero, and your front desk is about to feel the consequences.
Here's where it gets painful. Without updated insurance verification in place, your staff keeps collecting last year's copay amounts while the actual patient responsibility has ballooned. By the time the Explanation of Benefits arrives weeks later, you've already provided multiple sessions with hundreds of dollars in uncollected balances sitting on your books. Per patient.
The operational math is brutal. According to MGMA data, practices spend an average of 12.64 minutes manually verifying a single patient's eligibility. For a clinic seeing 40 patients daily, that's over eight hours of staff time, one full-time employee, essentially, dedicated to phone calls and payer hold music, and that's before you account for the errors that manual processes inevitably introduce.
But January doesn't have to mean revenue leakage, not if you're ready.
The shift from December to January isn't just a calendar flip, it's a complete financial reset for your patient population, and most of them have no idea until they see that first bill.
Think about the patient who hit her out-of-pocket maximum back in October. For the final months of the year, her therapy sessions cost nothing, zero. On January 1st, that same patient faces a deductible that could exceed $3,000 before insurance kicks in for anything beyond preventive care. If your team isn't armed with current benefit information, you're providing services on credit without knowing what you're actually owed.
The rise of High-Deductible Health Plans has made this exponentially worse, the IRS set the 2026 HDHP threshold at $1,700 for individual coverage. Out-of-pocket maximums now reach $10,150 for individuals and a staggering $20,300 for families. These aren't outliers anymore, HDHPs represent a huge chunk of employer-sponsored coverage, which means collecting from high-deductible patients has become a core skill rather than an occasional headache.
What makes January especially treacherous is the timing. Patients switch plans during open enrollment without telling their providers. They keep the same insurance carrier but move to a narrow network that quietly excludes your practice. Or they shift from a PPO to an HMO requiring referrals nobody obtained. Without systematic re-verification, these landmines don't surface until claims start bouncing back weeks after you've rendered services.
The denial rate data stopped me cold, industry surveys show that over 40% of providers now report denial rates exceeding 10%, with eligibility and registration errors ranking among the top culprits. And each denied claim costs real money to resolve, not just the lost revenue, but the staff hours burned on appeals and resubmissions.
The most effective defense against the January deductible reset happens before January arrives. Practices that build denial prevention into their December workflows avoid the worst of the post-holiday chaos.
Start with a batch eligibility review during the last two weeks of December. Pull your January appointment schedule and run eligibility checks on every patient. Most practice management systems support batch processing, and this single step identifies inactive policies, plan changes, and benefit updates before anyone walks through your door.
Real-time eligibility verification tools make this dramatically faster. Where manual verification takes those 12 minutes per patient, electronic verification returns results in seconds. The cost difference is equally striking. Research from CAQH found that 1,250 manual eligibility checks cost practices approximately $6,000 annually. The same volume of electronic checks? Around $1,000. That's an 83% reduction in verification costs alone, not counting time savings.
Next comes proactive patient outreach. And here's something that genuinely surprised me: text messaging has emerged as the most effective channel for reaching patients about insurance updates. Studies show SMS open rates hovering near 98%, with most patients responding within minutes. Compare that to phone calls, where nearly half of patients ignore calls from unfamiliar numbers. A simple December text campaign asking patients to upload photos of their new insurance cards can capture updated information before anyone's first appointment of the year.
Insurance card OCR technology takes this further. Modern optical character recognition doesn't just digitize card images. It extracts and validates policy numbers, group IDs, and payer information automatically. AI-powered OCR achieves extraction accuracy rates approaching 99%, eliminating the data entry errors that spawn denials. When a patient uploads a card photo through a secure link, the system populates your practice management software without human intervention.
Once you've collected updated insurance information, a structured verification checklist ensures nothing slips through. Professional associations including APTA and APA recommend confirming eight specific data points for every patient during the post-enrollment period:
Policy status comes first. Confirm the insurance is active for the specific date of service. Not just active generally, but valid on the exact day you'll see the patient.
Plan type matters for expectation-setting. Is this an HDHP, PPO, HMO, or narrow network plan? Each carries different cost-sharing structures and access requirements.
Deductible details require precision. What's the total annual deductible? How much has the patient already met? In January, that "met" amount is almost always zero.
Cost-sharing specifics vary more than many practices realize. Some plans use flat copays while others apply percentage-based coinsurance. A patient might owe $40 for primary care but 20% coinsurance for specialty services.
Network status deserves special attention after open enrollment. Confirm your in-network status for the patient's specific 2026 plan, not just their insurance carrier broadly.
Visit limitations catch practices off guard constantly. Many plans impose annual caps on therapy visits or require re-authorization after a certain number of sessions.
Prior authorization requirements often change between plan years. An authorization from 2025 may not carry over, and the new plan may have completely different approval criteria.
Out-of-pocket maximums help patients understand full-year exposure. Knowing when they'll hit the ceiling where insurance covers everything can actually encourage treatment compliance.
Armed with this information, your team can have transparent financial conversations before services are rendered. MGMA research consistently shows that practices with clear upfront communication about costs experience fewer billing disputes and higher collection rates.
High-deductible plans create a behavioral challenge that goes beyond verification mechanics. When patients see their January cost estimates, some will postpone or cancel appointments to avoid the expense. This happens constantly in therapy settings where care is ongoing.
The psychology makes sense. Paying $150 per session feels very different from paying $25, even when the annual total might be similar. Research suggests high deductibles cause many patients to delay non-urgent care, leading to worse outcomes and eventually higher costs.
Effective practices reframe the deductible as an investment rather than a penalty. The key message: front-loading deductible spending early in the year means lower costs for the remaining months. A patient who meets her deductible by March enjoys reduced expenses for nine months rather than facing high costs all year long.
Pointing patients toward their Health Savings Accounts or Flexible Spending Accounts can ease the immediate sting. HSA contribution limits for 2026 reach $4,400 for individuals and $8,750 for families. That's money specifically set aside for expenses like therapy copays and deductibles.
The goal isn't pressuring patients into care they can't afford, it's ensuring they make informed decisions based on accurate information rather than sticker shock from an unexpected bill.
The shift from manual to automated verification isn't about efficiency alone, it's about sustainability during your highest-volume periods.
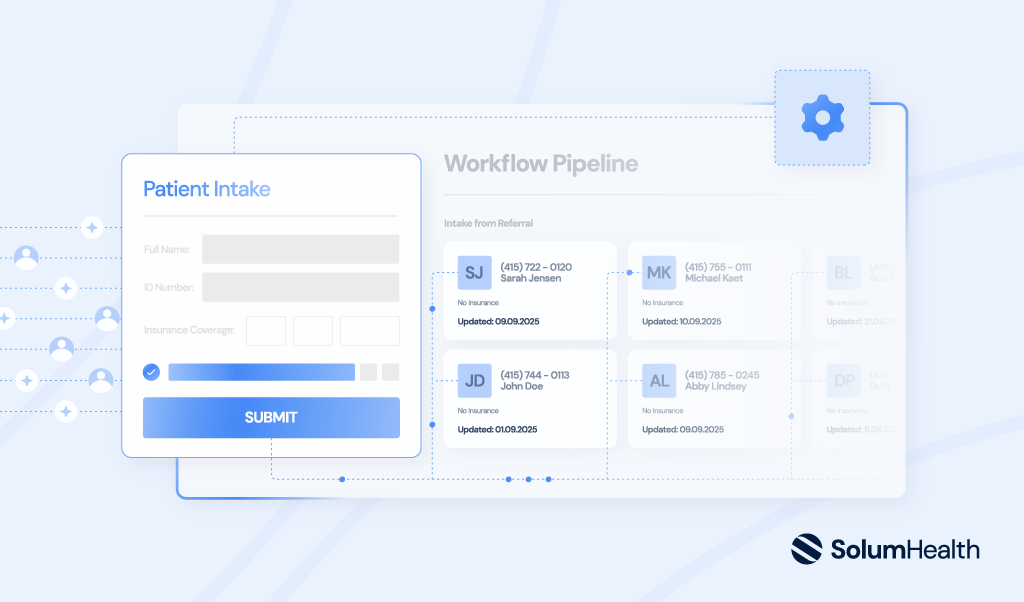
Electronic real-time eligibility checking eliminates the bottleneck that manual processes create during the January surge. Instead of staff spending hours on hold with payers, eligibility data flows directly into your practice management system. Discrepancies get flagged immediately rather than discovered weeks later on an EOB.
Insurance card OCR addresses data entry problems at their source. When patient information is captured photographically and extracted algorithmically, transcription errors largely disappear. Practices implementing AI-powered OCR report meaningful reductions in insurance-related claim denials.
The return on investment typically materializes within the first year. Between reduced staff hours, lower denial rates, and faster collections, operational savings often exceed technology costs. And automation scales in ways manual processes simply cannot. Whether you're seeing 40 patients daily or 400, electronic verification takes the same few seconds per patient.
Any technology handling patient insurance information must meet current privacy and security standards. HIPAA requirements continue evolving, with 2026 bringing notable updates including mandatory multi-factor authentication and stricter encryption requirements for protected health information.
When evaluating digital intake and verification platforms, look beyond basic compliance claims. Vendors should demonstrate specific technical safeguards appropriate for healthcare data. The shift toward verifiable security postures means practices bear responsibility for their technology partners' security practices.
So where does this leave you? The January deductible reset is coming whether you're ready or not. But the practices that build verification workflows now, invest in automation, and train staff on transparent financial conversations will weather the storm. The ones that don't will spend February chasing down uncollected balances and wondering where the revenue went.
I've seen both outcomes play out, year after year. The difference isn't luck. It's preparation.

For years, I managed a mental health practice with over 80 providers and more than 20,000 patients. Now, I’m building the tool I wish I had back then, AI automation that makes intake, insurance verification, and scheduling as seamless as running a healthcare practice should be.